Unlike most industries, where increased demand leads to rising costs for users, increasing engagement with healthcare actually drives down the overall cost of care.
If that sounds counterintuitive, consider:
- Many people don’t regularly engage with their healthcare providers due to fears about receiving bad news or fears about cost
- Delaying appointments may result in missing out on the benefits of an early diagnosis
- The longer a person stalls before receiving care, the more likely they will require numerous tests, treatments, and procedures
- Chronic or life-threatening health issues are more common among certain demographics, and treating these issues is expensive for not just patients and members, but also the healthcare industry as a whole
Given all this, it’s critical to focus on increasing engagement, especially among individuals who are in a rising or high-risk category. The more we can encourage these patients to be proactive with their health the better — not just from a health standpoint, but also from a financial one as well.
The problem is that increasing engagement is a challenge. The goal shouldn’t be to ensure people visit their doctor when problems become noticeable or unbearable, but instead, before they even realize they have a problem at all. Think about getting regular car maintenance versus waiting for the check engine light to come on.

Meeting individuals where they are
When we talk about barriers to care, we tend to get specific. We focus on costs or not being able to take time off from work or challenges in finding a doctor.
While these are all good areas to focus on, the real barrier is a much wider target: life is complicated.
Every one of us, regardless of our financial situation, experiences stumbles and roadblocks in our daily lives.
To really improve engagement, we need to understand what stumbles or roadblocks a person may be experiencing. Then we can work with the person to get around the barriers keeping them from being proactive about their health.
At apree health, a focus of ours has been to meet members where they are rather than hope they will be able to show up for an appointment with a provider.
Our emphasis is on communication. We want to take a micro approach, where we can reach out directly to rising or high-risk individuals to really understand what is keeping them from seeking preventive care.
The goal is to repeatedly get across four points:
- 1. We hear you and what you’re going through
- 2. We know there are things keeping you from getting care
- 3. Here’s why you should make your health a priority
- 4. Here’s how we’re going to make that easier
One benefit of this approach is that, when done consistently, it chips away at the excuses or objections an individual may have about visiting their provider. Another is that it starts the individual on a journey, one where their health is a priority.
Here’s an example of how that journey might look:
Say the patient is at risk for diabetes but hasn’t seen a provider in years. Through our conversations, we’ve identified two factors keeping them from scheduling an appointment.
One is the social impact, a feeling of embarrassment of being at risk for diabetes. The other is access or not being able to take time off from work for repeated visits.
Once we’ve identified these factors, we offer solutions.
Feeling embarrassed? Don’t worry, let’s connect you with one of our Care Guides to walk you through what you can expect during your visit and how addressing the problem today is the best option for you.
Can’t take time off from work for a visit? Here’s how you can access our virtual care, and how we can make it possible for you to talk with your provider, a clinician for behavioral health, and a health coach all in the same appointment.
Throughout this process, as the person moves through their journey, we also regularly celebrate wins and milestones. That way, the member is much more likely to stay engaged and positive as they go along.
Creating consistent touchpoints
The engines behind our micro approach to encouraging engagement are data and automation.
As we’ve piloted this program for rising or high-risk individuals, we’ve utilized the extensive data sets about our members. This data includes vital information about their claims, goals, propensity to engage, demographics, social determinants of health, and so on.
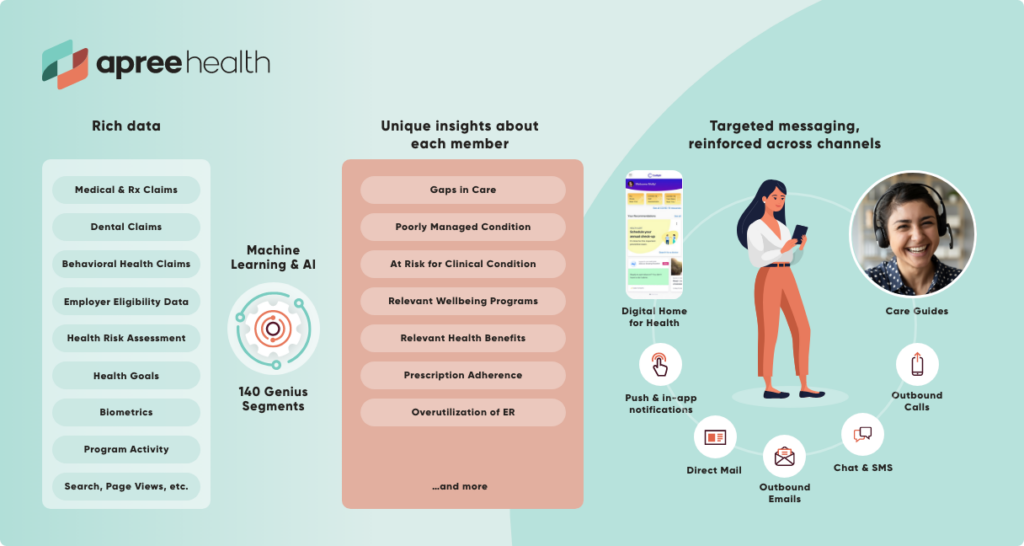
On the back end, we leverage automation to schedule and release touches to members, allowing us to scale outreach easily and keep touches on schedule.
The results have been extremely encouraging. Appointment scheduling has increased, as have digital engagements with features and programs that steer our members to care. Interactions with our Care Guides have also increased dramatically.
As we work to scale this approach, we’re excited to see where consistent touchpoints at the micro level can get us — and how getting those most at risk more engaged can help the industry as a whole.






